Immune Targets and Immunotherapy of Diabetes Mellitus
2021 marked the 100th anniversary of the discovery of insulin, which brought about a revolutionary change for individuals with type 1 diabetes. Prior to the discovery of insulin, diabetes meant a slow death, with adults typically surviving for less than two years and children rarely surpassing a year. Insulin therapy is the replacement or supplementation of insulin secretion for diabetes patients who suffer from an absolute lack or relative insufficiency of insulin secretion.
Insulin Becomes an Autoantigen
Since the first discovery of islet cell antibody (ICA) in serum from patients with type 1 diabetes in 1974, over 40 years of exploration has demonstrated that autoantibodies against islet cell proteins generally exist in the serum of patients with type 1 diabetes. The most significant and representative among them are insulin autoantibody (IAA), glutamic acid decarboxylase 65 kD autoantibody (GAD65AA), insulinoma antigen-2 autoantibody (IA-2AA), and zinc transporter-8 autoantibody (ZnT8AA). It is also clear that the existence of these islet cell autoantibodies not only aids in distinguishing between type 1 and type 2 diabetes, but also helps further differentiate between type 1A (autoimmune) and type 1B (idiopathic) diabetes. At the same time, it can also be used to predict whether type 1 diabetes will develop clinically based on the existence and mode of islet cell autoantibodies. Diagnosis of diabetes type is the premise of implementing correct treatment, especially type 1 diabetes. Early diagnosis or even prediction can enable appropriate interventions to preserve residual β-cell function, reducing the need for complete reliance on exogenous insulin. Therefore, screening high-risk groups, and even the general population, for islet cell autoantibodies may provide possibilities for early diagnosis and prevention of type 1 diabetes.
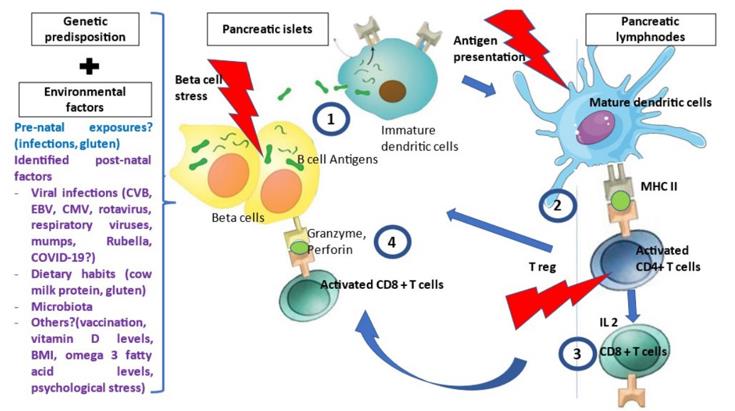 Fig.1 Pathophysiology of T1D.1,3
Fig.1 Pathophysiology of T1D.1,3
Targeting T cells in T1D
CD4+ and CD8+ T cells coordinate the inflammatory process, eventually destroying the islet β cells, leading to the occurrence of T1D. Many genes associated with susceptibility to type 1 diabetes are highly active in T cells. T cells infiltrate islets of diabetic patients, and diabetes can be transferred from one animal to another through adoptive transfer of T cells in a mouse model.
- Anti-CD3 immunotherapy: Preclinical studies have shown that short-term anti-CD3 therapy can induce disease remission in up to 80% of newly diagnosed diabetic non-obese diabetic (NOD) mice, which is associated with transient and partial T cell depletion. The fact that islet autoantibodies are produced years before diabetes onset presents an opportunity for therapeutic intervention. This chance has been exploited by administering Teplizumab to high-risk individuals with dysglycemia and the presence of 2 or more islet autoantibodies who had not yet been diagnosed with T1D. This research successfully delayed the development of T1D in these individuals.
- Antithymocyte Globulin (ATG): ATG is a polyclonal IgG that targets multiple T cell antigens and mediates cell depletion. Similar to anti-CD3 administration in NOD mice, ATG treatment was able to reverse diabetes in newly-onset mice. Preliminary small studies in patients with recent-onset T1D suggest that ATG treatment may help preserve β-cell function.
- CTLA-4-Ig fusion protein: Another example of T cell-directed immunotherapy is the CTLA-4-Ig fusion protein, which links the extracellular domain of human cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) to the modified Fc portion of human immunoglobulin G1 (IgG1). CTLA-4 is naturally highly expressed in regulatory T cells and interacts with the same ligands as the T-cell co-stimulatory receptor CD28, but with higher affinity. In a clinical trial, this fusion protein slowed the decline in β-cell destruction and function within an estimated 9.6 months.
- Immunosuppressive dimeric fusion protein: Immunosuppressive dimeric fusion protein is another Ig fusion protein containing two LFA-3 molecules that bind to the Fc portion of human IgG1. It binds to CD2 and mediates the depletion of antigen-experienced effector/memory T cells. this fusion protein inhibits the proliferation of T cells in mixed lymphocyte reactions in an Fc receptor-dependent manner.
- IL-2 therapy: Another immunotherapy approach targeting T cells involves the selective expansion of Tregs using the cytokine IL-2. The role of IL-2 in immune regulation suggests that defects in IL-2 or genes involved in IL-2 signaling are associated with autoimmune diseases, including T1D.
Targeting B cells in T1D
B cells are also involved in the development of T1D. In animal models, B cell deficiency or depletion inhibits diabetes onset. In addition, B cells act as effective antigen-presenting cells, capable of activating self-antigen-specific T cells, leading to diabetes. Anti-CD20 monoclonal antibody binds to CD20 expressed on the surface of B cells, resulting in their destruction through antibody-dependent cell-mediated cytotoxicity, apoptosis, and complement-dependent cytotoxicity.
Targeting Inflammatory Cytokines
- IL-1β: IL-1β secretion increases with the progression of diabetes and islet β-cell destruction.
- TNF-α: TNF-α has long been a target of interest in T1D. Studies in NOD mice yielded mixed results, suggesting that TNFα exerts site-specific, cell-type-specific, and age-dependent effects.
- IL-21: IL-21 is also an attractive target for T1D immunotherapy. IL-21 is a characteristic cytokine produced by T follicular helper cells (Tfh cells), assisting in B cell antibody production, thus playing a crucial role in humoral immunity. Lack of IL-21 or IL-21 receptor in NOD mice prevents diabetes development, and transgenic expression of IL-21 in non-autoimmune-prone mice is sufficient to induce diabetes..
Microbial Derived Therapy
Environmental factors such as gut bacterial composition are crucial for shaping immune responses and modulating T1D susceptibility. Changes in bacterial composition are also associated with the development of early β-cell autoantibody responses. Currently, microbial-derived therapeutics for T1D are in early stages of development and require more work to determine whether they can be harnessed to modulate immune response and provide long-term clinical benefits.
References
- Houeiss, Pamela, Sandrine Luce, and Christian Boitard. "Environmental triggering of type 1 diabetes autoimmunity." Frontiers in Endocrinology 13 (2022): 933965.
- Pearson, James A., Eoin F. McKinney, and Lucy SK Walker. "100 years post-insulin: immunotherapy as the next frontier in type 1 diabetes." Immunotherapy Advances 1.1 (2021): ltab024.
- Distributed under Open Access license CC BY 4.0, without modification.
